Employee health
Healthier businesses start with better employee health and well-being
Smarter investment in employee health can deliver sustainable, long-term value for both your company and your employees. And among a competitive, rapidly changing world and labor force, protecting that investment is more important than ever.
Many employers focus on reactive health solutions that emphasize “sick care” and managing high-cost claims. But this approach often misses opportunities to address employee health in a more personal, cost-effective and forward-thinking way.
We’ve found that when companies proactively support employee well-being with solutions tailored to all corners of their diverse and unique workforces, they’re rewarded with employees who are healthier overall, actively using their health plan’s services, programs and tools. Through simpler experiences and stronger member support that’s designed to deliver better results, we’ll partner with you to find the approach that works best for your company and employees.
Employee health is a continuum that needs proactive, holistic support
Over time, the health of your employees changes and evolves. With good health comes high satisfaction and productivity, along with lower overall health care costs. However, when there’s need for care, the trend reverses: Satisfaction and productivity dip, while care costs rise. This pattern resembles a curve – what we like to call the care experience curve.
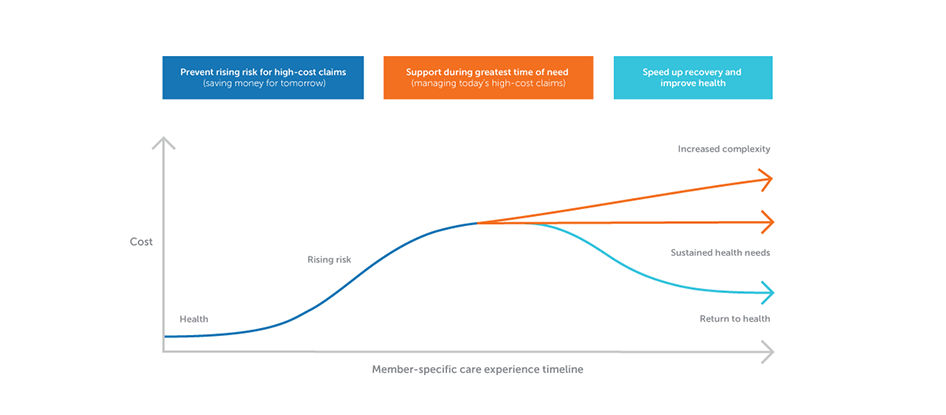
Through analyzing this curve, we’ve found that many high-cost health conditions don’t happen suddenly. Instead, they build across weeks, months and years. Companies that focus on just the peaks of need (and the peaks of cost) miss opportunities to approach the curve earlier. By providing support at all stages, companies can help flatten the care experience curve, treating (and perhaps even preventing) conditions and issues before they create higher health plan costs.
This focus on flattening the curve is the true “value” in your health plan’s value-added services, like health and well-being programs, medical and behavioral disease management, case management, and more. When deployed correctly, these services work in harmony with traditional benefit offerings (like medical, pharmacy and dental), acting seamlessly to give you and your workforce the tools, support and motivation needed to improve employee health.
At HealthPartners, we’re differentiated by teams, processes and technology. Our solutions are designed to help you address the specific needs of your employees at every stage of their care experience curves. We do this by connecting dots across rising health risks, conditions, care gaps and social determinants of health (like access to quality health care, education, food, social support and safe living environments) to reduce health disparities. Then, we identify and engage employees at the right time and place.
In other words, we offer:
- Advanced predictive algorithms to address rising risks sooner
- A meaningful, personalized experience for each employee that’s both comprehensive and connected
- Care and plan teams working together, sharing data and enabling more proactive approaches to managing care and cost
When these approaches come together, they can reduce the likelihood of high-cost care visits and improve workforce health, resulting in sustainable value and

Comprehensive employee health and wellness solutions for all needs
Having a range of workforce health and well-being solutions is important. But do yours partner to meet the needs of your employees along their care experience curve journeys? We’ve found that when employee health solutions and benefit plans work together – supported by aligned teams, technology and processes – they consistently deliver the results necessary to prevent high-cost visits.
That’s why our solutions follow evidence-based population health metrics – backed by our
We search for answers with a holistic view of both physical and mental health, capturing claims and clinical data alongside factors like social determinants, life satisfaction measures and healthy lifestyle behaviors – issues that can create gaps in care and inequalities in treatment when overlooked.
This comprehensive framework informs every aspect of how we bring our health solutions together. Our robust analytics and predictive modeling help ensure that we’re reaching out to and supporting our members with meaningful interventions before health issues become larger problems.
Helping employees stay healthy and reduce health risks
- Preventive care reminders and support: Personalized, multichannel communication campaigns that encourage preventive care and reduce care gaps at the right times
- Health and well-being digital tools and programs: Online and mobile support through an online account – as well as personalized coaching options – helps make mental, physical, emotional, social, spiritual and financial health goals easier to achieve
- 24/7 CareLineSM and BabyLine phone service: Registered nurse support for any need, with special resources for pregnant or new parents
- Nurse NavigatorSM program: Registered nurse support to help employees understand their care options and make the best decisions for their needs
Employee Assistance Program (EAP) : Virtual and in-person resources to help employees feel and work their best- Occupational medicine services: Pre-placement testing, ergonomics consulting,
onsite flu and vaccination clinics , and much more
Support for employees with complex and chronic needs
- Behavioral Health Navigators and Pharmacy Navigators: Dedicated experts help members navigate benefits coverage for emotional health, answering questions and connecting employees to relevant care and medication resources
- Inpatient case management: In-hospital support to ensure a timely, safe discharge, plus transition support after a hospital stay to help prevent readmission
- Complex case management: Outpatient support for multiple conditions to improve self-management, reduce complications, avoid hospital readmissions and lower the need for high-cost care
- Medical and behavioral disease management: Condition management for behavioral health and medical diagnoses, helping prevent and delay rising risk

Collaboration, identification and communication that make a difference
Everyone on our health plan teams – from Member Services to our care navigators to our disease and case management teams – seamlessly partners to create healing relationships for every member, every day.
It’s a process that starts well before a claim arrives to us from the doctor’s office. Instead, it happens right when a need occurs, in real time, as our teams and predictive algorithms identify crucial care times in a member’s health journey. For example:
- When there’s an emergency care visit or hospitalization, a new diagnosis or medication prescribed, or other health risk identified in electronic health records (EHRs)
- When a health assessment identifies a rising health risk like hypertension, obesity or substance use
- When there’s a need for a preventive screening based on demographic data or health histories
When we see these opportunities, our multichannel, personalized approach reaches members in ways that are meaningful to them. Convenient, tailored outreach tactics connect them to tools, resources and support via their preferred communication method and easy-to-use online account. We carefully use our existing claims, demographic and health history data to ensure all outreach is relevant, relatable, responsive and – most importantly – effective.

Coverage that uniquely partners with providers to create better health outcomes
Our proactive approach to better employee health and lower costs also includes what could be the most vital collaboration of all: partnerships with doctors, nurses, specialists and caregivers.
Many health plans simply incentivize doctors to better manage conditions and improve health outcomes. Those strategies matter, but we’ve found it takes deeper engagement to drive the approaches necessary for meaningful improvement. That’s why our health plan teams serve as an extension of an employee’s care team, working directly with providers to give support before, during, after and between doctor visits.

A key part of this relationship involves using EHR technology to work together with care teams. Our EHR connections to local, regional and national health systems make it easier to communicate and collaborate about each member’s needs in real time. That helps us sooner understand care patterns and potential rising risks, resulting in treatment plans that better align our members, their plans and their care teams.
Then, our condition and case management nurses establish a shared, trusted partnership alongside the employee and their care team. We help the employee better understand their condition, make better treatment decisions, improve self-management and education, and facilitate community referrals. Members are always placed firmly at the center of our communication – we use motivational interviewing and clinical decision-making techniques to holistically identify needs and help them meet their goals.
It all results in action that proactively addresses potential care gaps and offers health equity. Plus, relationships that help employees return to better health (and the workplace) sooner.
A proven approach to employee health and wellness
Low administrative fees make some plans look attractive, but they don’t account for long-term value. Instead, true, sustainably lower care costs (and better bottom-line results) come from proactive involvement in employee health – made possible by technology, processes and collaboration between health plans and health care teams.
This strong care and coverage collaboration led us to create
Those partnerships also influence how we create our plan networks, helping us identify the best care systems that champion affordability and quality. Ultimately, these strategic, intentional measures and relationships help members see clinical improvements sooner, reducing higher-cost claims over time and bolstering your bottom line.
For example, in our plans, appropriate antidepressant medicine use is 10% higher (Healthcare Effectiveness Data and Information Set 2020, relative to national average). And when high-risk members across our plans are more engaged in our health advocacy programs:
- Diabetes optimal care rates are 3.5% higher per engaged high-risk member
- Heart disease optimal care rate is 10% higher per engaged high-risk member
- Case management post-discharge follow-up is 31% higher
- Emergency room costs for core chronic conditions (asthma, COPD, CAD, diabetes, heart failure) are 7% lower
- Emergency room costs for complex conditions are 5% lower
- Hospitalization costs for core chronic conditions (asthma, COPD, CAD, diabetes, heart failure) are 29% lower
- Hospitalization costs for cancer are 4% lower
